Showing Xiao Yao San the Door?

The Breakup Series: Xiao Yao San and alternatives
Rumor has it that Xiao Yao San is the most prescribed Chinese Medicine herbal formula in the U.S. All I ask is go easy on me if I’m wrong. However, it does seem like a popular remedy. (Hey, it’s a breakup series. There has to be an Adele reference somewhere.)
Whether it’s called Rambling Powder or Free & Easy Wanderer, Xiao Yao San is commonly used to calm stress and anxiety, which is running rampant in society these days.
It tends to be safe and has a wide range of applications. But is this always the best formula to partner up with when your patient needs to chill out?

Historical Precedents + Formula Comparisons
Xiao Yao San first came onto the scene in 1107. There are three schools of thought on its origins.
Is it a:
- variation of Si Ni San (Frigid Extremities Powder)?
- modification of Dang Gui Shao Yao San (Tangkuei and Peony Powder)?
- combination of both formulas?
I’m not going to pick sides. (Rarely a good idea in relationship dustups!) Instead, I’ll discuss what herbs the formulas have in common.
Xiao Yao San is a Liver-Spleen harmonizing formula that addresses the pattern of Liver constraint with Blood deficiency and a frail Spleen. It treats Qi stagnation, Blood and Qi deficiency, and Dampness.
Si Ni San is also a formula that regulates and harmonizes the Liver and Spleen. It is used for the pattern of Yang- or hot-type inversion due to internal constraint of Yang Qi. This formula is used for excess conditions and focuses on treating Qi stagnation.
In contrast, Dang Gui Shao Yao San is a Blood regulating formula. But it also treats Liver-Spleen disharmony. In this case, the pattern involves Blood stasis and Qi stagnation due to Dampness. The formula focuses on treating Blood deficiency and Dampness.
Xiao Yao San shares Si Ni San’s approach of treating Qi stagnation by using Chai Hu to spread Liver Qi in order to relieve Liver constraint. Both formulas also contain Bai Shao and Zhi Gan Cao to nourish Liver Blood, tonify the Spleen, and moderate spasms.
Both Dang Gui Shao Yao San and Xiao Yao San address Blood Deficiency with the combination of Dang Gui and Bai Shao. The two formulas strengthen the Spleen and dry Dampness with the dui yao of Bai Zhu and Fu Ling.
Unique to Xiao Yao San is the inclusion of Bo He and Wei Jiang (baked fresh ginger) which were traditionally prepared as a draft to take the main powdered ingredients with. Bo He enhances Chai Hu’s ability to relieve Liver constraint and any heat associated with it. Wei Jiang is an envoy that harmonizes the Stomach and prevents rebellious Qi from developing.
Xiao Yao San Indications
One of the keys to having an effective relationship with Xiao Yao San is understanding its indications. The formula targets a mixture of excess and deficiency. You’re looking for signs and symptoms of Liver Qi constraint combined with Spleen Qi and Blood deficiency.
Some of the excess signs and symptoms from constraint could include:
- hypochondriac pain
- abdominal pain
- breast distention
- headache
- bitter taste in the mouth
- dry mouth and throat due to heat
- wiry pulse
Note: for more heat signs such as increased irritability, red eyes, palpitations, or heavier menses, Jia Wei Xiao Yao San would be the preferred formula. It includes the addition of Zhi Zi and Mu Dan Pi to clear heat..
The concurrent Spleen and Blood Deficiency is reflected in:
- fatigue
- reduced appetite
- irregular menses
- pale tongue
- deficient pulse
Xiao Yao San isn’t designed to treat a purely excess or deficient disorder. The tonifying herbs may create stagnation and heat in excess conditions. In more deficient cases, the acrid herbs may prove to be too moving and drying*
While there might be a spark of attraction, in the end, the flame will peter out.
*In a case like this, especially if there’s more pronounced Blood Deficiency, Dang Gui Shao Yao San could be a good alternative...
What do you do when the most popular chill formula ends up being a dud? You look to see who’s waiting in the wings...
Excess Patterns
When playing the field, it helps to narrow down the options. To start with, we’ll look at two excess patterns for constraint and their recommended formulas:
- constraint due to stagnant Qi (Yue Ju Wan)
- constraint and clumping of Liver Qi (Chai Hu Shu Gan San)
Yue Ju Wan
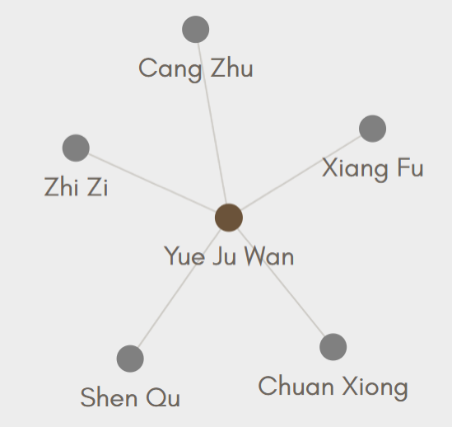
Yue Ju Wan and its creator, Zhu Dan-Xi, figure prominently in the history of constraint in Chinese Medicine. "Constraint," by the way, is a term that has been interpreted and re-interpreted over the centuries.
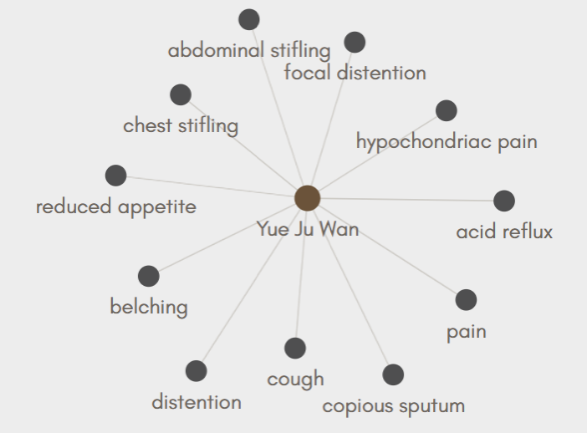
Zhu Dan-Xi’s intention in creating Yue Ju Wan was for it to be a flexible formula that treats different types of constraint arising from Qi stagnation. This could be due to emotional excess, irregular eating, or excessive cold or heat exposure.
Yue Ju Wan regulates the flow of Qi with particular emphasis on unblocking the ascending and descending flow of Qi in the middle burner. Ongoing constraint of the Qi dynamic can give rise to a number of disorders which this formula is designed to address.
Each herb in the formula targets a different aspect and individual doses can be increased or decreased according to their prevalence:
- Cang Zhu - targets the Spleen and Stomach and dries Dampness and transforms Phlegm
- Chuan Xiong - moves Blood and alleviates fixed pain
- Xiang Fu - resolves constrained Qi and helps unblock the Qi dynamic
- Zhi Zi - clears any heat or fire that has developed
- Shen Qu - reduces food stagnation and helps harmonize the Stomach
For the patient who has an excess presentation with multiple disorders that stem from constraint of the Qi dynamic, Yue Ju Wan might be the flexible partner they’re looking for
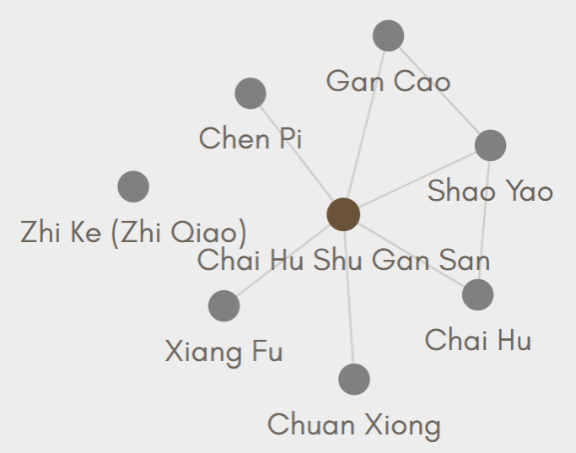
Chai Hu Shu Gan San
If you really like the family, Xiao Yao San isn’t the only offspring of Si Ni San who can tackle frustration, deep sighing, and suppressed emotions.
For Liver Qi constraint in a patient without deficiencies, Chai Hu Shu Gan San could be the perfect match. This is the date who’s direct, straightforward, and gets to the point. In fact, it’s contraindicated for long-term use.
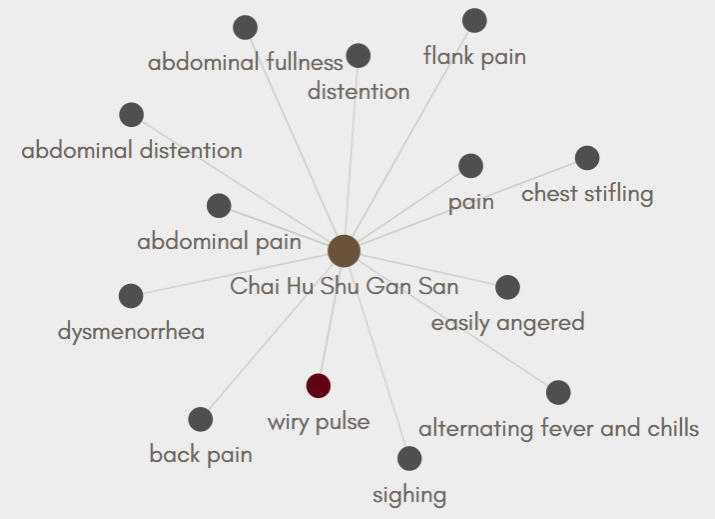
Chai Hu Shu Gan San has the same trio of Chai Hu, Bai Shao, and Zhi Gan Cao that Xiao Yao San contains. They spread Liver Qi, nourish the Blood to soften the Liver, and alleviate pain.
To further address constraint and stagnation in the Liver Channel, Xiang Fu and Chuan Xiong have been added. Chen Pi and Zhi Ke will help move middle burner Qi and direct Qi downward to offset ascending Liver Qi.
This is for the person who’s been biting their tongue while tolerating an ongoing stressful situation. Chest stifling, hypochondrial and flank pain, abdominal discomfort accompanied by belching, being easily angered, and a wiry pulse are indications that Chai Hu Shu Gan San is worth hooking up with...
Deficiency Patterns
Perhaps the prior two formulas are too bold and brash. The kind of date you can’t get a word in edgewise with. They wear you out with all their energy.
This might be the time to look to see who’s hanging out in the corners or against the wall...
Yi Guan Jian
Maybe the patient still has a mix of deficiency and excess. But no matter how many times you try, it’s clear Xiao Yao San is never going to make it beyond the friend zone. Kind of like the couple that everyone thinks would be perfect for each other but somehow doesn’t quite connect.
In this situation, some practitioners recommend pivoting to Yi Guan Jian.
Pattern Comparison
Comparing Xiao Yao San and Yi Guan Jian is a bit like using a looking glass that’s a little warped. They’re not pure mirror images, but there’s definitely overlap.
Xiao Yao San treats Liver constraint with underlying Blood Deficiency and a weak Spleen. It’s often used for cases where emotional disharmony contributes to the constraint. The primary focus is to relieve the Liver constraint while secondarily nourishing the Qi and Blood deficiencies.
Yi Guan Jian treats Liver and Kidney yin deficiency with qi stagnation. In this case, the yin deficiency may lead to constraint and cause emotional disharmony like irritability. Here, the primary focus is on tonifying Liver and Kidney yin to soften the Liver, relieving constraint is secondary.
*There are times when fire from constraint may lead to yin deficiency. Yi Guan Jian could still be appropriate to use in this situation.
The middle jiao organs are involved in both scenarios:
- for Xiao Yao San, a weak Spleen contributes to blood deficiency, dampness, fatigue, and a reduced appetite;
- with Yi Guan Jian, the Stomach is attacked by the Liver leading to possible epigastric pain and distention plus acid reflux.
The level of constraint vs deficiency and the degree of the deficiency will influence the presenting signs and symptoms. Here again, both formulas show indications such as:
- a deficient, wiry pulse
- some degree of redness on the tongue
- dryness, especially of the mouth and throat
- hypochondriac pain
Those who’d benefit from Yi Guan Jian may have a more rapid pulse, more intense dryness, and a redder tongue. There could be signs of Kidney deficiency like a weak and sore lower back.
Herbal Approach
Where things really start to look different is in the formula compositions. The only herb the two formulas have in common is Dang Gui for tonifying and moving blood.
With Yi Guan Jian, there’s an emphasis on tonifying Yin and moistening the fluids, which will allow Qi to move more freely.
Gou Qi Zi, from the tonify blood category, is the chief herb. It nourishes both the Liver and its mother, the Kidney, enriches yin, and is moistening, which facilitates movement.
The three assistants help address the root disorder of yin deficiency. Sheng Di Huang clears heat, nourishes yin, and generates fluids. Sha Shen (often Bei Sha Shen) and Mai Men Dong both tonify Stomach and Lung yin. This not only treats the parched mouth and throat, but it facilitates the downward directing action of both organs and helps counterbalance the Liver.
Chuan Lian Zi is used to disperse the secondary condition of constrained Liver qi and its resulting pain and heat. It also helps moderate the cloying tendency of the other herbs in the formula.
But what if the Liver isn’t the major player?

How about the person who’s extremely deficient? Who no longer has the reserves to tolerate the minor irritations of life?
Someone with an undernourished Heart? (Too many breakups perhaps?)
This could be the time for:
Zhi Gan Cao Tang
Zhi Gan Cao Tang comes from the category of formulas that tonify Qi and Blood. A heart that’s deficient in Qi and Blood has lost its vitality.
This can manifest as:
- palpitations
- anxiety
- pale tongue
The pulse is thin and weak, sometimes to the point of irregularity.
With diminished Heart Blood, the Shen has lost a place to comfortably reside. This can lead to irritability and insomnia. Fluids might also be affected causing a dry mouth, throat, and constipation.
The antithesis of Chai Hu Shu Gan San, Zhi Gan Cao Tang is complex, takes its time, and is supposed to be ingested for at least 10 days before determining whether it’s a good fit (Bensky et al., 2004).
Ingredients
Zhi Gan Cao nourishes the Heart and tonifies middle burner Qi. Sheng Di Huang nourishes Heart Yin and tonifies the Blood. These two ingredients have the largest dosages in the formula.
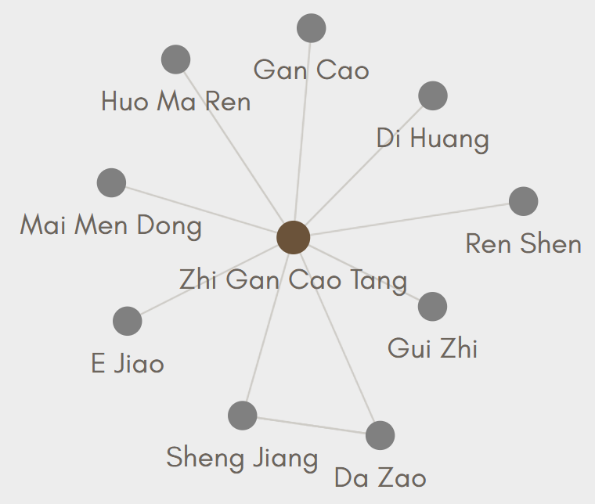
As additional Qi tonifiers, Ren Shen and Da Zao help calm the Shen and strengthen the Spleen to further support the Heart and generate new Blood. They assist Zhi Gan Cao in its functions.
To further assist Sheng Di Huang in enriching the Yin and moistening dryness, E Jiao, Mai Men Dong, and Huo Ma Ren have been added to the formula. E Jiao also further tonifies the Blood.
Gui Zhi unblocks Heart Yang. Sheng Jiang strengthens the Stomach so the formula can be more easily digested. Rice wine is added at the end of the decoction to enhance the circulation.
Final Thoughts
For some people, Xiao Yao San is the One and Only formula. It’s a perfect fit.
However, if nothing seems to be working, it might be time for the four words that no one in a partnership likes to hear. “We need to talk.”
To talk about formulas like Si Ni San, Dang Gui Shao Yao San, Yue Ju Wan, Chai Hu Shu Gan San, Yi Guan Jian, Zhi Gan Cao Tang...
And to talk about lifestyle changes, stress management techniques, setting boundaries, secondary gains, and possibly making difficult life decisions.
Because in the end, there are some situations that no herbal formula can solve on its own.
~ Dr. Susan D. West, DACM
Bensky, D., Clavey, S., & Stoger, E. (2004). Chinese herbal medicine: Materia medica (3rd edition). Eastland Press, Inc.